The Revenue Cycle Challenges Facing Pain Management Groups
And What to Do About Them
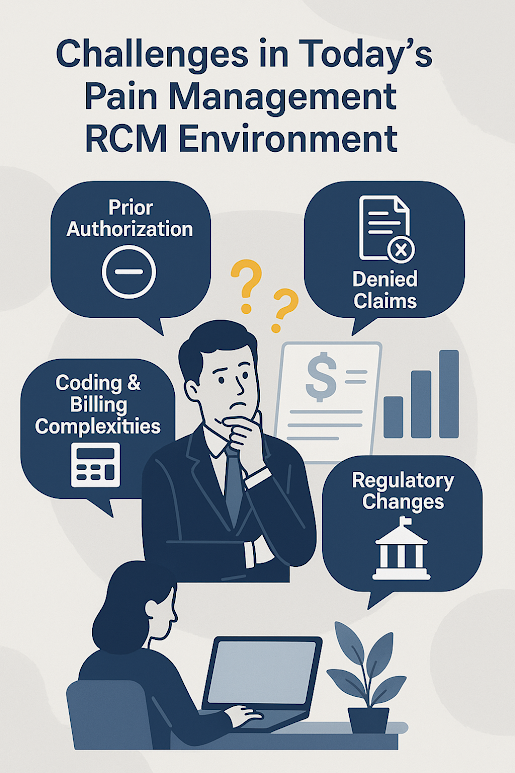
Pain management groups play a vital role in treating patients with chronic and acute pain using a combination of interventional procedures, physical therapy, medication management, and advanced diagnostics. But while these groups focus on delivering relief and restoring quality of life, many are increasingly burdened by the complexity and inherent challenges of their revenue cycle operations.
At the heart of the issue is a perfect storm of diverse payer types, evolving billing rules, and administrative strain, all of which put pressure on practice’s ability to thrive. Let’s review some of these challenges and consider ways to manage them more effectively, now and in the future.
A Complex Reimbursement Landscape
Unlike many other specialties, pain management groups often operate across three very different reimbursement models:
• Commercial Insurance: While these plans offer relatively stable reimbursement rates, they often come with strict documentation requirements, procedure authorizations, and narrow networks.